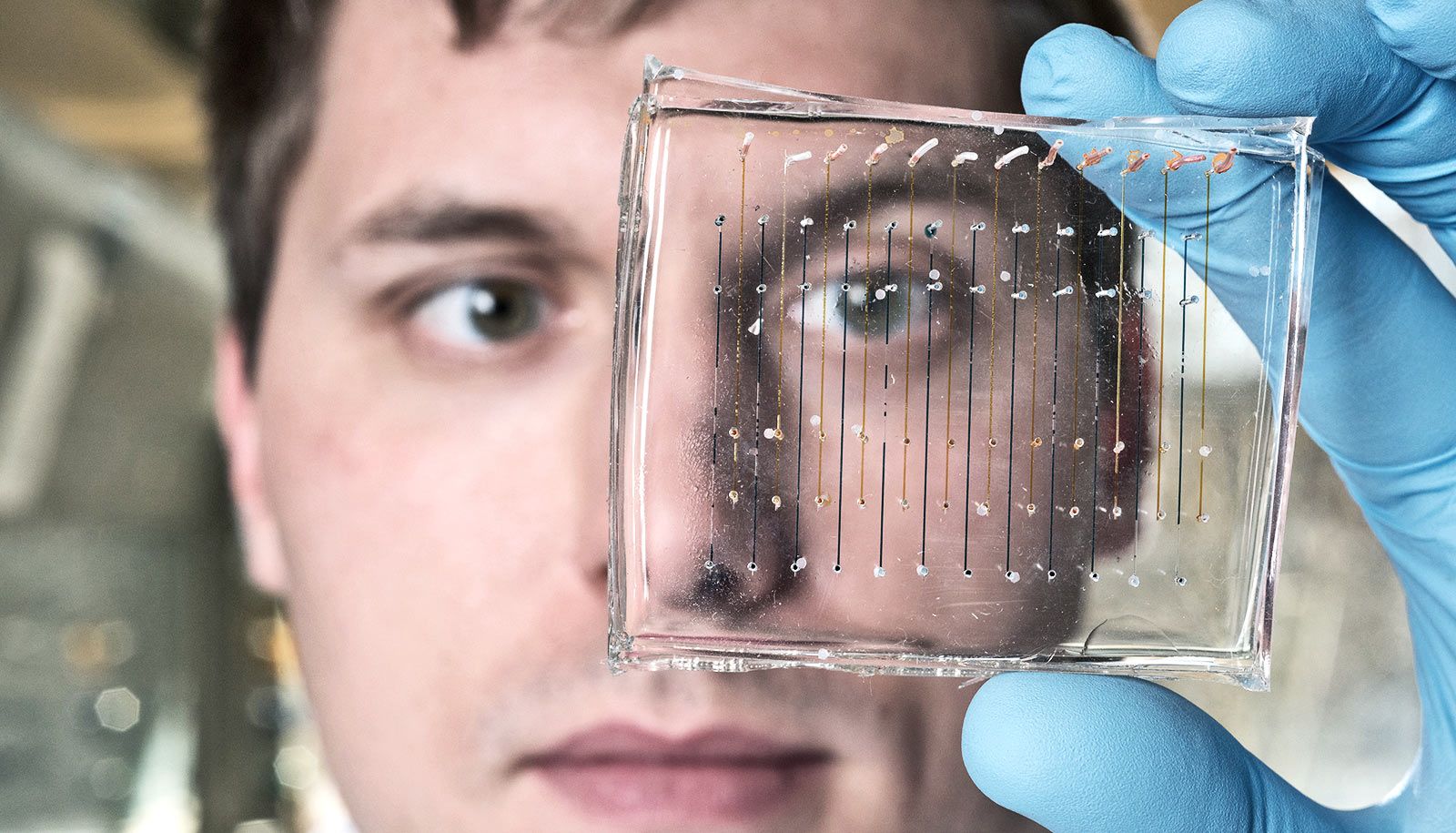
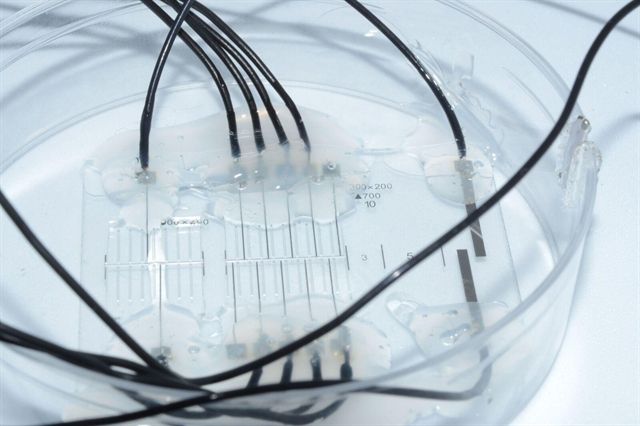
Rutgers scientists have created a tiny, biodegradable scaffold to transplant stem cells and deliver drugs, which may help treat Alzheimer’s and Parkinson’s diseases, aging brain degeneration, spinal cord injuries and traumatic brain injuries.
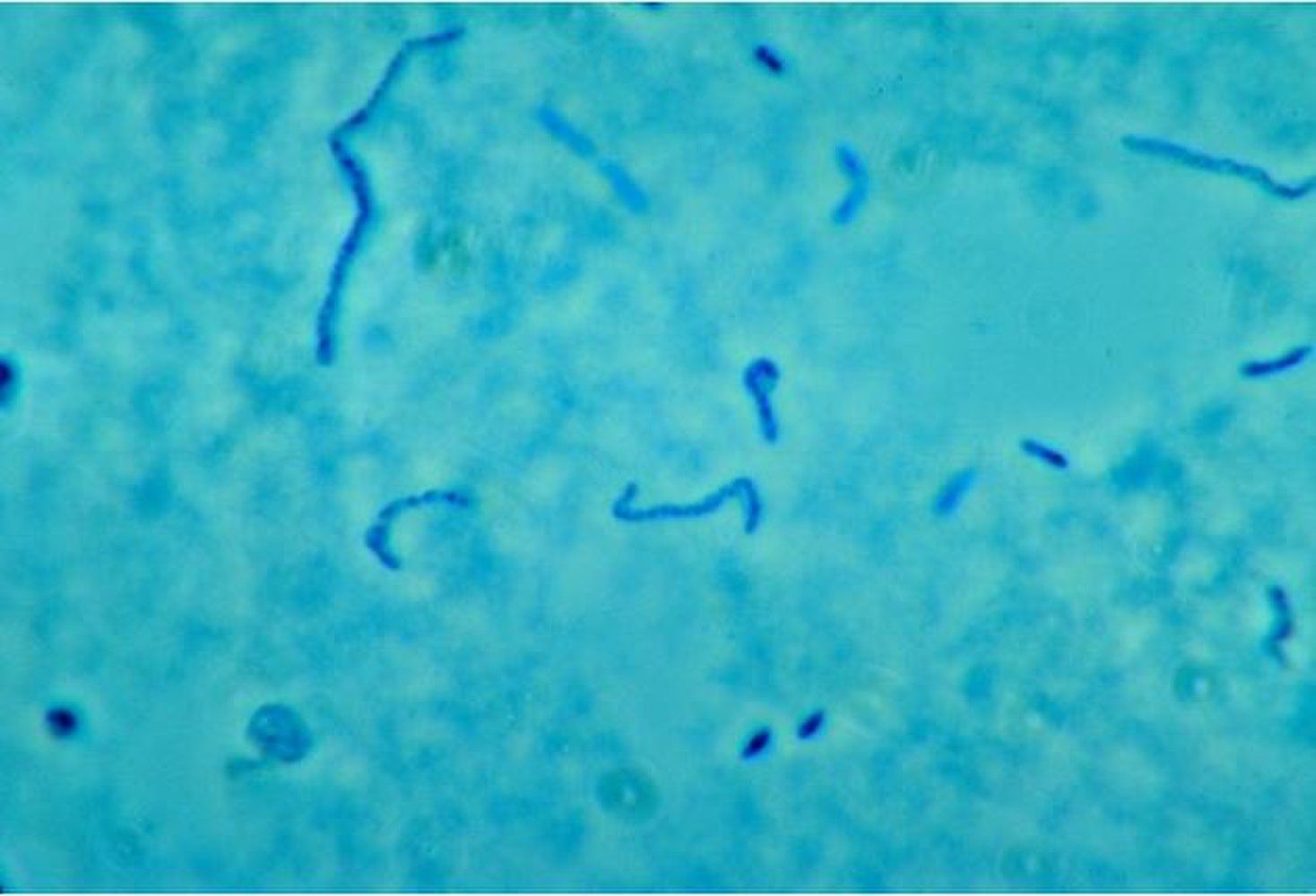
Stem cell transplantation, which shows promise as a treatment for central nervous system diseases, has been hampered by low cell survival rates, incomplete differentiation of cells and limited growth of neural connections.
So, Rutgers scientists designed bio-scaffolds that mimic natural tissue and got good results in test tubes and mice, according to a study in Nature Communications. These nano-size scaffolds hold promise for advanced stem cell transplantation and neural tissue engineering. Stem cell therapy leads to stem cells becoming neurons and can restore neural circuits.