An aggressive blood pressure target of under 120 mm Hg can significantly reduce heart disease risk, researchers found. Despite more side effects and higher costs, the approach proved cost-effective and beneficial for many patients.


Australian researchers have used an innovative genome-wide screening approach to identify genes, and their encoded proteins, that play critical roles in the prevention of lymphoma development, revealing new potential treatment targets for these blood cancers.
The study, published in Nature Communications, has identified a group of proteins known as the GATOR1 complex as essential tumor suppressors.
The GATOR1 complex normally functions as a “brake” on cellular growth by regulating pathways that control cell growth and metabolism. When GATOR1 components are lost or defective, this protective mechanism fails, allowing cells to grow uncontrollably.
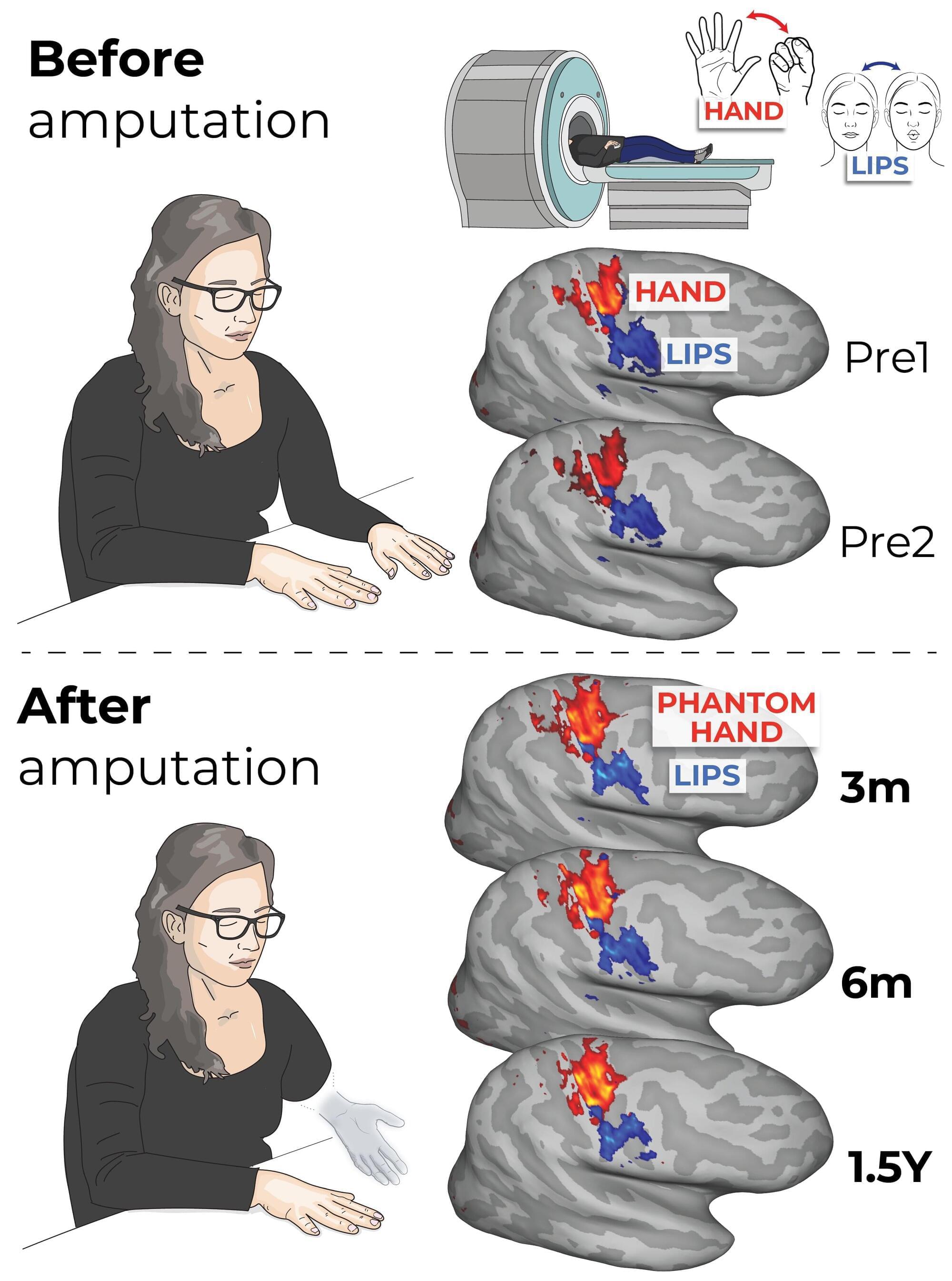
The brain holds a “map” of the body that remains unchanged even after a limb has been amputated, contrary to the prevailing view that it rearranges itself to compensate for the loss, according to new research from scientists in the UK and US.
The findings, published in Nature Neuroscience, have implications for the treatment of “phantom limb” pain, but also suggest that controlling robotic replacement limbs via neural interfaces may be more straightforward than previously thought.
Studies have previously shown that within an area of the brain known as the somatosensory cortex there exists a map of the body, with different regions corresponding to different body parts.

Researchers can use a metric called the particle number concentration (PNC) to calculate the number of particles in a sample, such as the number of marbles in a jar.
Researchers at the National Institute of Standards and Technology (NIST) have developed a new mathematical formula to calculate the concentration of particles suspended in a solution. The new approach, which yields more accurate results than current methods, can be used to deliver the correct drug dosage to patients, measure the amount of nanoplastics in ocean water, and help ensure the correct level of additives in food products, among other applications.
The researchers have published their findings in Analytical Chemistry.
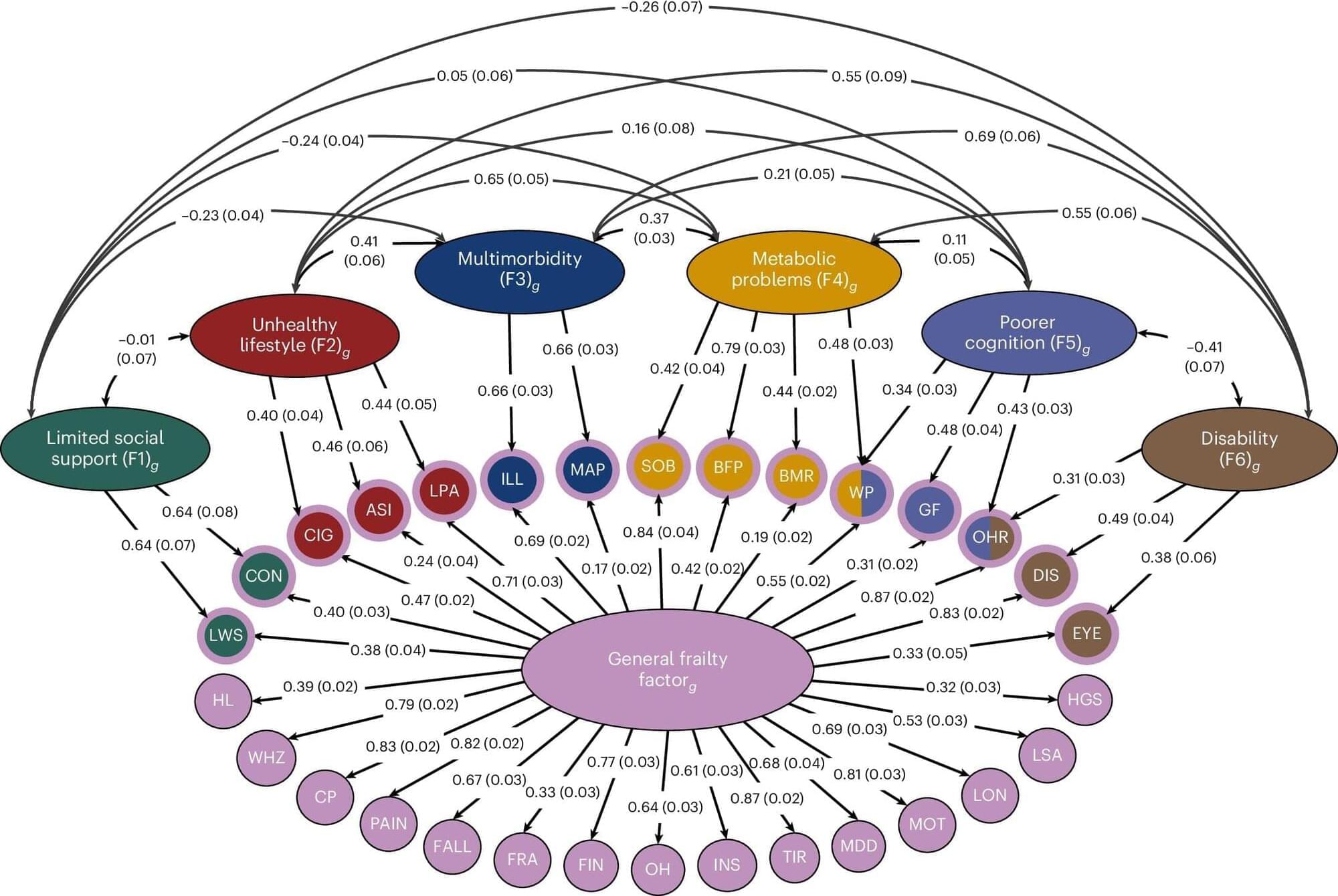
It’s a fact of life: Some people age better than others. Some ease into their 90s with mind and body intact, while others battle diabetes, Alzheimer’s or mobility issues decades earlier. Some can withstand a bad fall or bout of the flu with ease, while others never leave the hospital again.
New University of Colorado Boulder-led research, published in Nature Genetics, sheds light on why that is.
In it, an international team of co-authors identifies more than 400 genes associated with accelerated aging across seven different sub-types. The study reveals that different groups of genes underlie different kinds of disordered aging, a.k.a. frailty, ranging from cognitive decline to mobility issues to social isolation.

Paralysis from spinal injury has long remained untreatable. Could scientific developments get people affected on their feet again sooner than imagined? In a worldwide first, Tel Aviv University researchers have engineered 3D human spinal cord tissues and implanted them in a lab model with long-term chronic paralysis, demonstrating high rates of success in restoring walking abilities. Now, the researchers are preparing for the next stage of the study, clinical trials in human patients.

Harvard researchers developed liquid crystal elastomers that can switch between multiple shapes — chevrons, flat layers, and coils — in response to heat.
By aligning molecules in different directions, the material can be programmed to morph into domes, saddles, or fin-like motions inspired by stingrays and jellyfish.
The shape-shifting material could advance applications in soft robotics, biomedical devices, and smart textiles.
Liquid crystal elastomers are a class of soft materials that can change shape in response to stimuli such as light or heat — making them promising for applications in soft robotics, wearable and biomedical devices, smart textiles and more. But designing compositionally uniform elastomers that can change into different shapes in response to just one stimulus has been challenging and has limited the application of these potentially powerful materials.
Now, researchers from the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) have developed a way to program liquid crystal elastomers with the ability to deform in opposite directions just by heating — opening up a range of applications.
The research was published in Science.
(May be a repost from 2024)
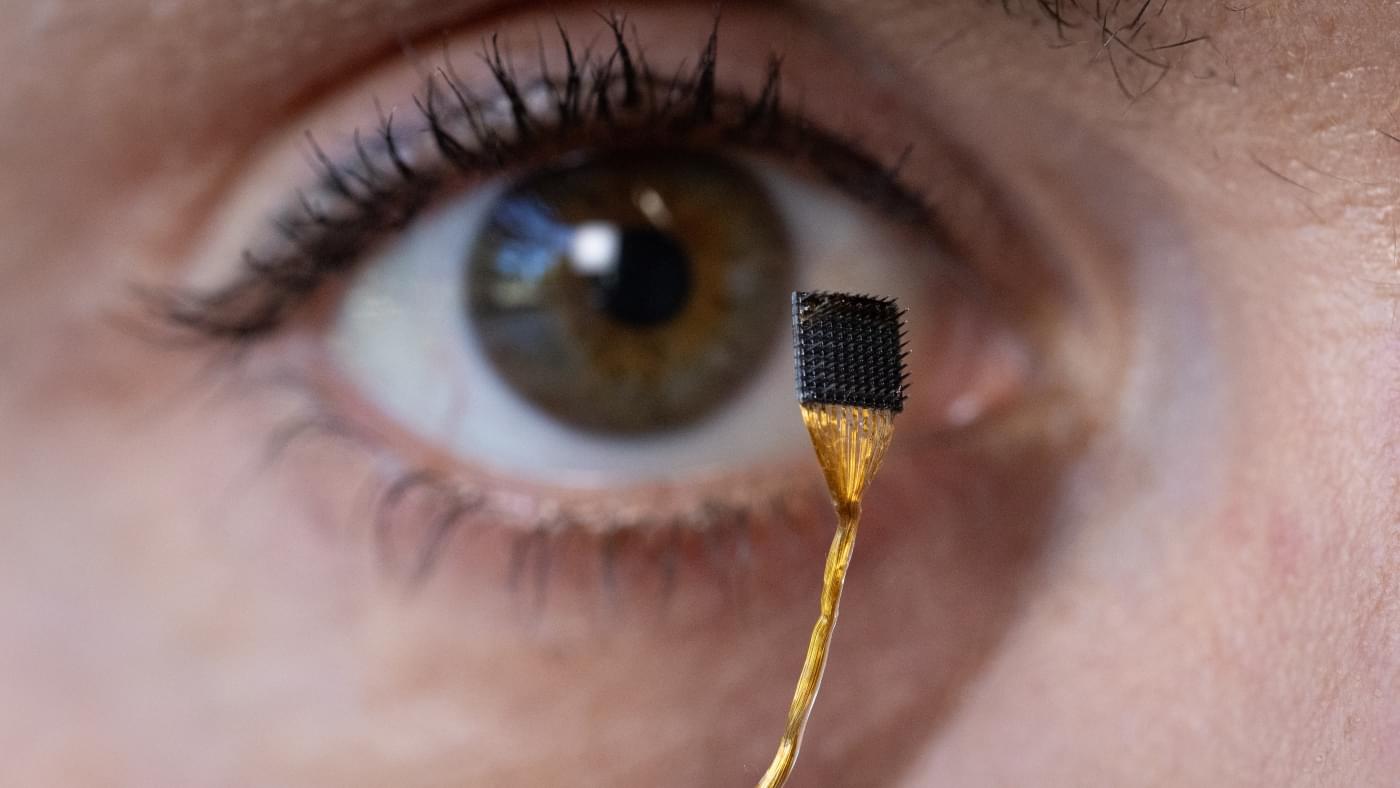
Having lived with an ALS diagnosis since 2018, Kate Nycz can tell you firsthand what it’s like to slowly lose motor function for basic tasks. “My arm can get to maybe 90 degrees, but then it fatigues and falls,” the 39-year-old said. “To eat or do a repetitive motion with my right hand, which was my dominant hand, is difficult. I’ve mainly become left-handed.”
People like Nycz who live with a neurodegenerative disease like ALS or who have had a stroke often suffer from impaired movement of the shoulder, arm or hands, preventing them from daily tasks like tooth-brushing, hair-combing or eating.
For the last several years, Harvard bioengineers have been developing a soft, wearable robot that not only provides movement assistance for such individuals but could even augment therapies to help them regain mobility.
But no two people move exactly the same way. Physical motions are highly individualized, especially for the mobility-impaired, making it difficult to design a device that works for many different people.
It turns out advances in machine learning can create a more personal touch. Researchers in the John A. Paulson School of Engineering and Applied Sciences (SEAS), together with physician-scientists at Massachusetts General Hospital and Harvard Medical School, have upgraded their wearable robot to be responsive to an individual user’s exact movements, endowing the device with more personalized assistance that could give users better, more controlled support for daily tasks.