This new brain scan may spot Alzheimer’s early—but it doesn’t work the same for everyone.
Category: neuroscience – Page 78

Neuroscientists remain steadfastly uncertain about how the brain encodes memory
Researchers from Monash University, in collaboration with the European Biostasis Foundation and Apex Neuroscience, have revealed that although most neuroscientists agree that long-term memories depend primarily on neuronal connectivity patterns, significant uncertainties persist regarding precisely how these memories are structurally encoded.
Brains can retain memories for days, months and even across a lifetime of decades, through mechanisms that remain elusive to those at the cutting edge of neuroscience. Long-term memory enables animals to shape behaviors by linking past experiences with present contexts.
There are fragile memories, like recalling the name of someone you just met, or the location of where the keys were set down, that can seemingly escape the brain’s data capture. And there are durable memories that can survive periods of global neuronal inactivity and disruption, indicating that ongoing neural activity is not required to maintain stored information.

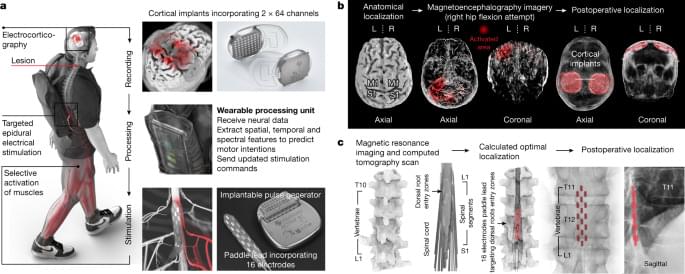
Low-intensity brain stimulation may restore neuron health in Alzheimer’s disease
Alzheimer’s disease (AD) is a debilitating neurodegenerative condition that affects a significant proportion of older people worldwide. Synapses are points of communication between neural cells that are malleable to change based on our experiences. By adding, removing, strengthening, or weakening synaptic contacts, our brain encodes new events or forgets previous ones.
In AD, synaptic plasticity, the brain’s ability to regulate the strength of synaptic connections between neurons, is significantly disrupted. This worsens over time, reducing cognitive and memory functions and leading to reduced quality of life. To date, there is no effective cure for AD, and only limited treatments for managing the symptoms.
Studies have shown that repetitive transcranial magnetic stimulation (rTMS), a noninvasive brain stimulation technique that uses electromagnetic pulses to target specific brain regions, has therapeutic potential to manage dementia and related diseases. From previous studies, we know that rTMS can promote synaptic plasticity in healthy nervous systems. Moreover, it is already used to treat certain neurodegenerative and neuropsychiatric conditions. However, individual responses to rTMS for AD management are variable, and the underlying mechanisms are not clearly understood.
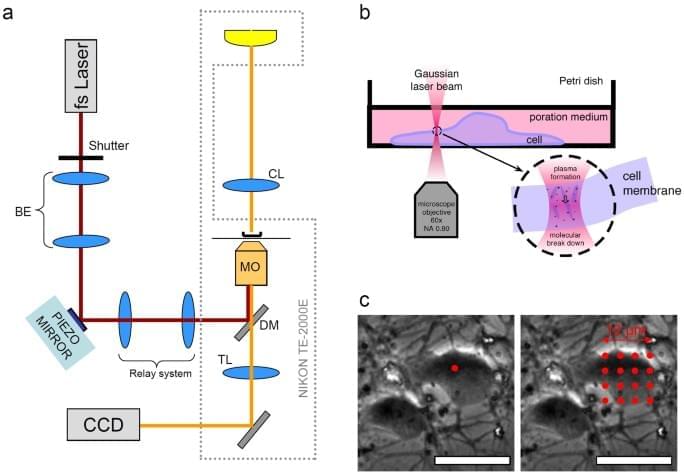
Fast targeted gene transfection and optogenetic modification of single neurons using femtosecond laser irradiation
Year 2013 face_with_colon_three Basically this is the light based nanotransfection version that can eventually be put on a simple smartphone or smartwatch that can be an entire hospital in one touch healing the entire body in one touch or just areas that need healing.
Antkowiak, M., Torres-Mapa, M., Witts, E. et al. Sci Rep 3, 3,281 (2013). https://doi.org/10.1038/srep03281
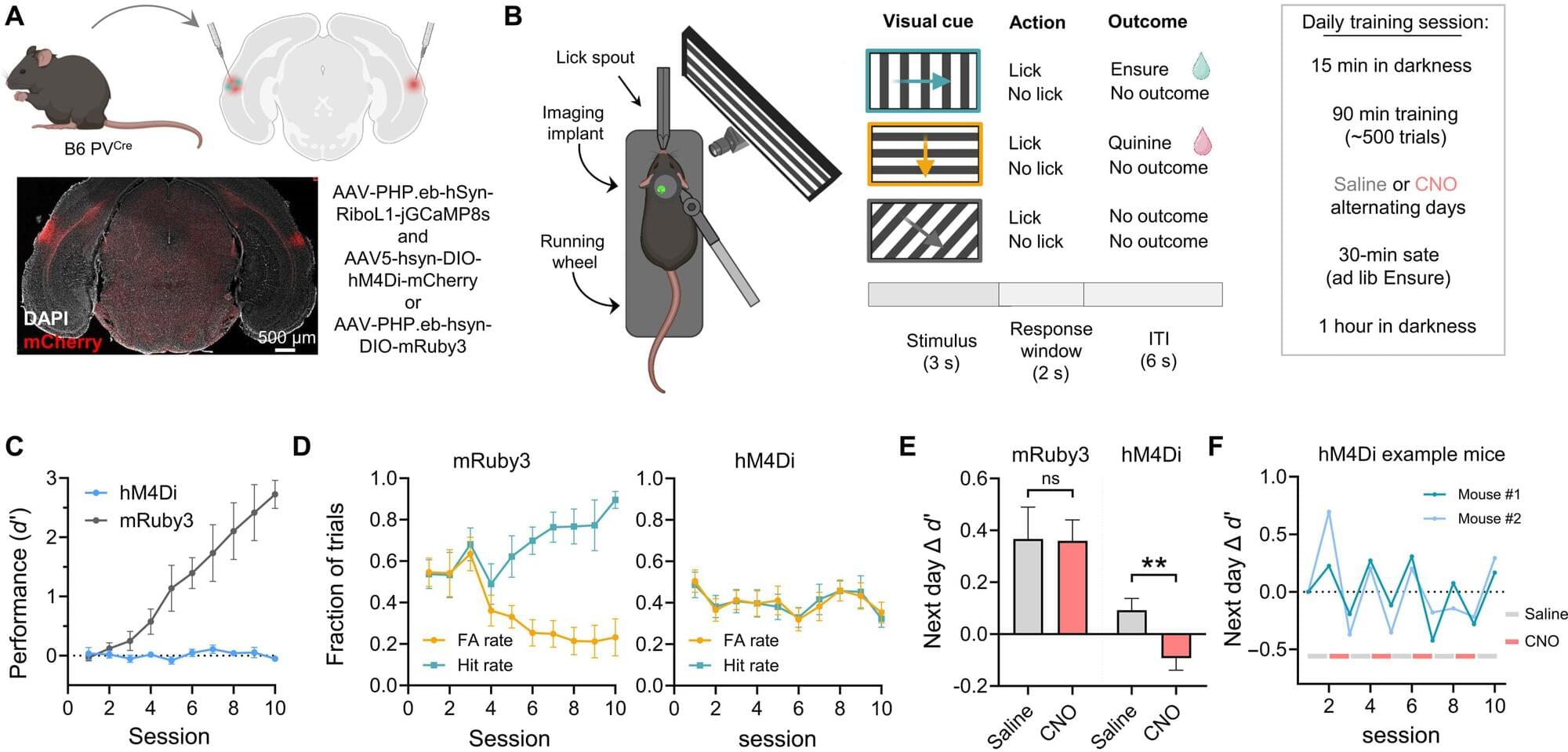
How key brain cells help replay and store memories during rest and sleep
How does the brain store knowledge so that you actually remember what you have learned the next day or even later? To find out, researchers at the University of Oslo disconnected one type of nerve cell in the brain of mice while the animals rested after having learned something new. This gave new answers to what actually happens when you remember earlier experiences for later use. The study is published in the journal Science Advances.
In the first phase of this experiment, mice were trained to recognize that an image with a particular pattern meant that they would be given a reward in the form of a sweet drink. Two different groups of mice were then put in front of a computer screen where they were able to see several images containing different patterns. In order to demonstrate that they remembered which image led to a reward, the mice had to lick a small “nozzle” that dispensed the drink.
While the mice performed this action, researchers at the University of Oslo monitored the activity in their brain cells using a special microscope. “It took some time before the mice understood which pattern triggered a reward. We could see what was happening with their neurons while they mastered the task,” says researcher Kristian K. Lensjø, who works at the Institute of Basic Medical Sciences and the Department of Biosciences at the University of Oslo.
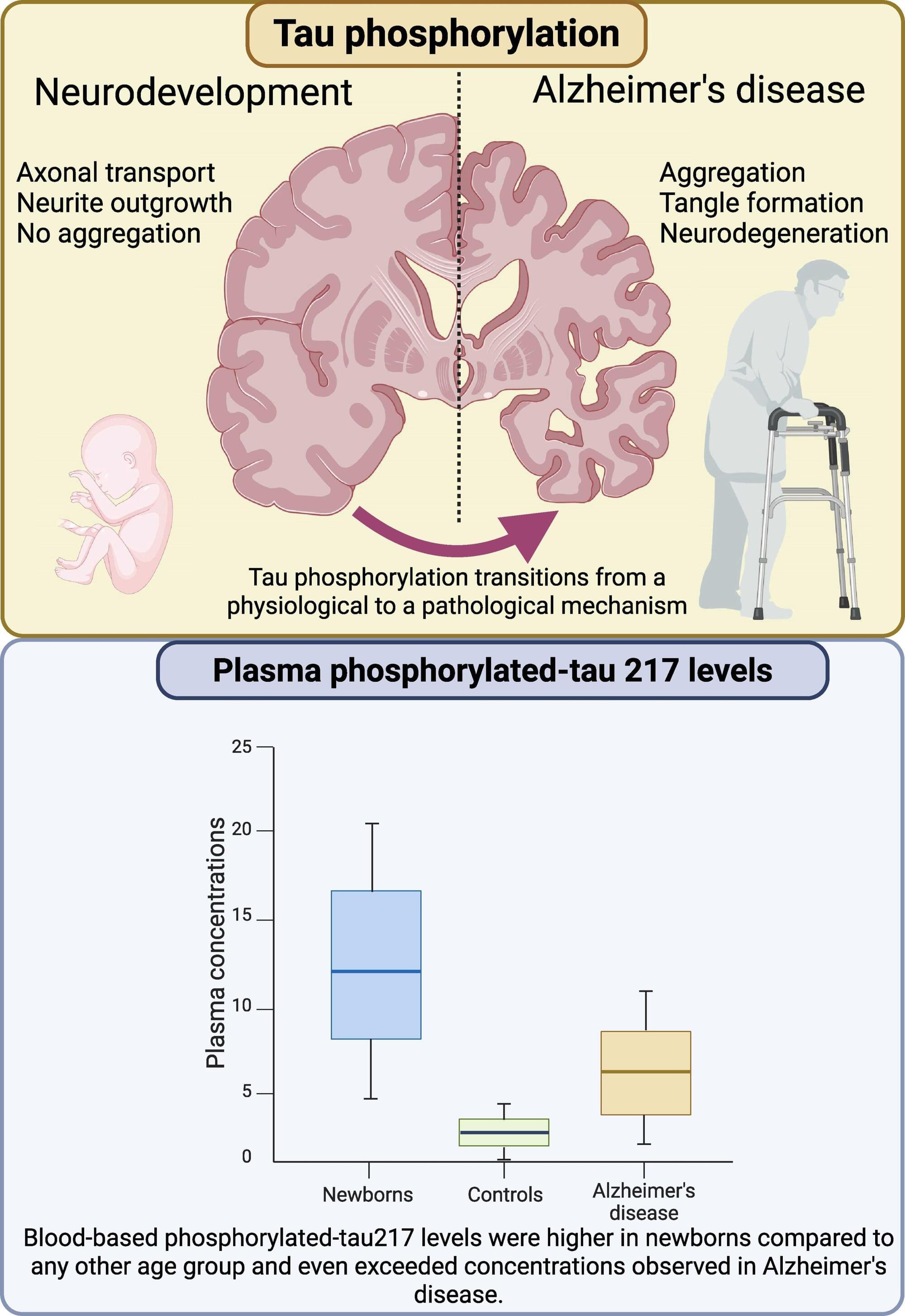
Newborns have elevated levels of a biomarker for Alzheimer’s
Newborn babies and patients with Alzheimer’s disease share an unexpected biological trait: elevated levels of a well-known biomarker for Alzheimer’s, as shown in a study led by researchers at the University of Gothenburg and published in Brain Communications.
First author Fernando Gonzalez-Ortiz and senior author Professor Kaj Blennow recently reported that both newborns and Alzheimer’s patients have elevated blood levels of a protein called phosphorylated tau, specifically a form called p-tau217.
This protein has largely been used as a diagnostic test for Alzheimer’s disease, where an increase in p-tau217 blood levels is proposed to be driven by another process, namely the aggregation of b-amyloid protein into amyloid plaques. Newborns (for natural reasons) do not have this type of pathological change, so interestingly, in newborns increased plasma p-tau217 seems to reflect a completely different—and entirely healthy—mechanism.

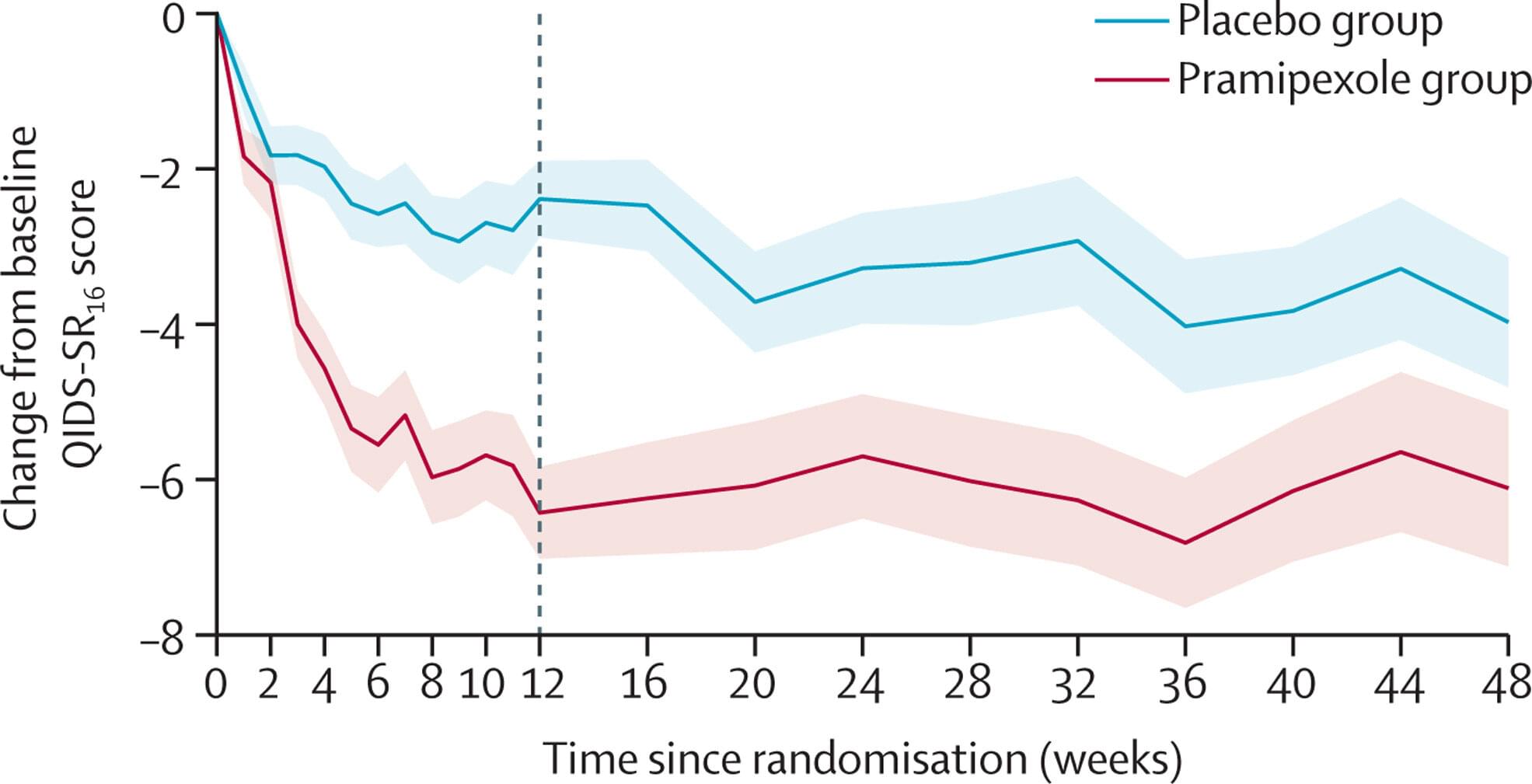
Parkinson’s drug reduces symptoms in treatment-resistant depression, clinical trial finds
A drug used for Parkinson’s disease has been shown to be effective in reducing the symptoms of difficult to treat depression, according to a study led by the University of Oxford.
In the largest clinical trial to date, pramipexole was found to be substantially more effective than a placebo at reducing the symptoms of treatment-resistant depression (TRD) over the course of nearly a year, when added to ongoing antidepressant medication.
The trial, published in The Lancet Psychiatry, included 150 patients with treatment-resistant depression, with equal numbers receiving 48 weeks of pramipexole or a placebo, alongside ongoing antidepressant medication.
